What Is a Sleep Study and Why Is It Important?
What exactly is a sleep study? A sleep study Melbourne appointment, formally known as a polysomnogram, is a non-invasive diagnostic test that monitors your body’s functions while you sleep. Medical professionals rely on sleep testing Melbourne services to accurately diagnose sleep disorders such as obstructive sleep apnea, chronic snoring, and periodic limb movement disorder.
This comprehensive assessment tracks multiple physiological signals simultaneously throughout the night. During sleep testing Melbourne, adhesive sensors are placed on the scalp, face, chest, fingers, and legs to monitor brain activity (EEG), eye movements (EOG), muscle tone (EMG), heart rhythm (ECG), breathing patterns, blood oxygen levels, body position, and leg movements. Collecting this data together provides a complete picture of how your body functions during sleep.
Why does accurate diagnosis matter so much? Untreated sleep disorders can lead to serious long-term health risks, not just daytime fatigue. Conditions identified through sleep testing Melbourne may increase the risk of:
- Heart disease and other cardiovascular conditions
- High blood pressure
- Stroke
- Workplace and driving accidents due to impaired alertness
- Reduced work performance and productivity
A professionally conducted polysomnogram during sleep testing Melbourne delivers the detailed insights specialists need to develop an effective, personalized treatment plan. Overnight monitoring captures sleep patterns that short clinic visits cannot detect, enabling doctors to identify the exact type and severity of the disorder. This level of precision ensures patients receive targeted treatment rather than generic recommendations that may fail to address their specific sleep condition.
What Types of Sleep Studies Might They Encounter in Melbourne?
Melbourne sleep clinics offer several distinct types of sleep studies, each designed for specific diagnostic or treatment purposes. The most common is a diagnostic sleep study, which identifies conditions like obstructive sleep apnea, snoring patterns, and periodic limb movement disorder through comprehensive overnight monitoring.
1. Diagnostic Sleep Study
A diagnostic sleep study identifies conditions like obstructive sleep apnea, snoring patterns, and periodic limb movement disorder through comprehensive overnight monitoring.
2. Therapy Sleep Study
A therapy sleep study compares sleep activities during active treatment to assess how interventions are working. This type helps clinicians understand whether current treatments effectively address the underlying sleep disorder.
3. CPAP Titration Studies
CPAP titration studies (or BPAP titration) determine the optimal air pressure settings for patients who require airway support devices. During this specialized study, technologists adjust pressure levels throughout the night to find the most effective setting that keeps airways open without causing discomfort.
4. Multiple Sleep Latency Tests and Maintenance of Wakefulness Tests
Multiple Sleep Latency Tests measure daytime sleepiness by recording how quickly someone falls asleep during scheduled nap opportunities. Maintenance of Wakefulness Tests assess treatment efficacy by evaluating a patient’s ability to stay awake in quiet, comfortable conditions.
Hospital-Based vs Home-Based Sleep Studies
In-clinic overnight studies take place in private bedrooms with ensuite facilities at hospitals or dedicated sleep centers. A Sleep Technologist monitors recordings throughout the night via low-light video cameras and intercom systems, providing immediate assistance if sensors become dislodged or patients need bathroom breaks.
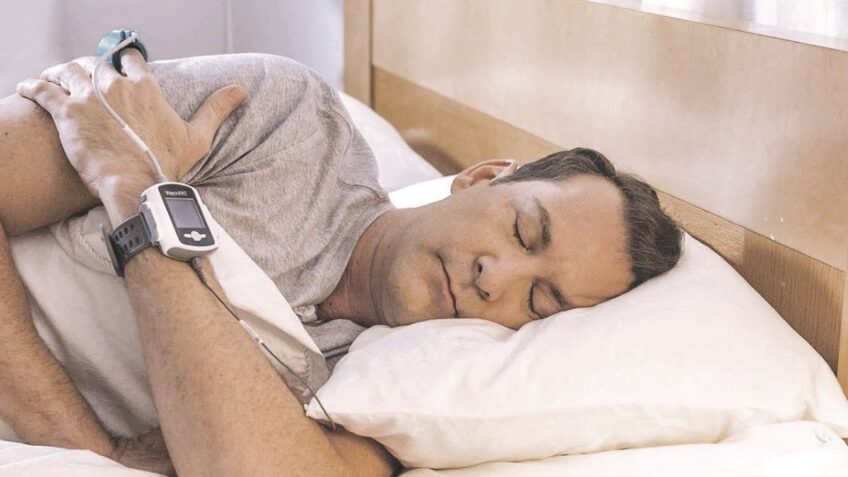
Home-based sleep studies use portable monitoring equipment that patients take home after initial setup at the clinic. These studies typically measure fewer parameters than full polysomnograms but offer convenience for those with mobility issues or scheduling constraints. Patients return the equipment the following day for data analysis.
The choice between hospital and home studies depends on:
- Suspected condition severity
- Need for real-time monitoring
- Medical complexity
- Patient mobility and comfort preferences
- Insurance coverage requirements
Home studies work well for straightforward obstructive sleep apnea diagnosis, while complex cases requiring detailed brain wave monitoring or immediate intervention benefit from supervised clinic environments.
How Should They Prepare Physically Before the Appointment?
Physical preparation directly impacts the accuracy of sleep study results. The sensors and monitoring equipment work best when applied to clean, product-free skin, making proper hygiene before sleep study essential for reliable data collection.
Shower and Hair Care Requirements
A thorough shower on the day of the appointment removes oils, dirt, and residue that interfere with sensor adhesion. Hair should be freshly washed and completely dry before arrival. Avoid applying any hair products including gel, mousse, hairspray, or leave-in conditioners. These products create a barrier between scalp sensors and the skin, potentially compromising brain wave readings during the study.
Skin Preparation Guidelines
Clean, bare skin ensures optimal sensor contact throughout the night. The pre-sleep study preparation checklist includes:
- Remove all makeup, including foundation, powder, and eye makeup
- Skip moisturizers, lotions, and body oils on the face, chest, and legs
- Avoid applying deodorant or antiperspirant
- Remove nail polish from at least one finger for the oxygen saturation monitor
- Shave facial hair if possible, as it may affect sensor placement
Medication Guidelines for Sleep Studies
Continue taking all prescribed medications as usual unless specifically instructed otherwise by the referring doctor. This includes:
- Regular prescription medications at their scheduled times
- Blood pressure medications
- Heart medications
- Diabetes medications
Sleep medications present a special consideration. Some doctors prefer patients take their usual sleep aids to replicate typical sleeping conditions, while others request avoiding them. Confirm medication guidelines with the sleep clinic when booking the appointment.
What to Wear and Bring
Comfortable, loose-fitting sleepwear allows for sensor placement and unrestricted movement. Two-piece pajamas work better than nightgowns or one-piece outfits, as sensors attach to the chest and legs. Pack a change of clothes for the morning and any toiletries needed for the post-study shower.
What Lifestyle Habits Should They Avoid Before the Sleep Study?
Caffeine avoidance before sleep study
It is crucial to avoid caffeine on the day of the appointment. This includes coffee, tea, energy drinks, soft drinks, and chocolate, all of which contain caffeine that can disrupt natural sleep patterns and delay the onset of sleep. The stimulating effects of caffeine can last 4-6 hours, making it challenging for technologists to obtain accurate baseline sleep data.
Alcohol restrictions
Alcohol should be restricted for at least 24 hours before the study. Although alcohol may initially make you feel drowsy, it actually disrupts the structure of your sleep by breaking up sleep cycles and suppressing REM sleep. This creates a false representation of your usual sleep patterns, potentially hiding or altering symptoms that doctors need to observe.
No naps policy
Patients are required to stay awake throughout the day leading up to their appointment. Napping during the day reduces sleep pressure, making it more difficult to fall asleep during the study. Patients who nap may experience longer time taken to fall asleep or lighter stages of sleep, which compromises the quality and reliability of diagnostic data.
Avoidance of makeup, hair products, and skin lotions
Before coming to the clinic, patients should refrain from using makeup, hair products, and skin lotions. These substances create a barrier between sensors and skin, resulting in poorer quality electrical signals being captured during monitoring. Oil-based products are particularly problematic for EEG electrodes that measure brain wave activity.
Heavy meal restrictions
Patients should avoid heavy meals close to bedtime; however, they should not arrive hungry either. Having a light dinner 2-3 hours before the study allows for comfortable sleep without any digestive discomfort or hunger pangs that may disrupt natural sleep patterns.
Excessive exercise limitations
Engaging in excessive exercise in the evening prior to the study can raise body temperature and adrenaline levels, making it difficult to fall asleep at the scheduled time. While light activity is acceptable, intense workouts should be completed earlier in the day.

How Should They Mimic Their Typical Night’s Sleep During the Study?
Should they stick to their normal bedtime routine?
Yes, maintaining regular bedtime habits during the sleep study is essential for obtaining accurate diagnostic results. The goal is to replicate a typical night as closely as possible, allowing sleep specialists to observe genuine sleep patterns rather than artificially altered behavior.
What specific routines should they follow?
Patients should arrive at the sleep clinic having followed their usual evening routine. If they normally read for 20 minutes before bed, they should bring a book. If they typically watch television to wind down, most Melbourne sleep clinics provide this option in their private rooms. The key is consistency with their typical night routine for sleep study purposes.
Does their usual sleep position matter?
Sleep position plays a significant role in accurate diagnosis, particularly for conditions like obstructive sleep apnea. Patients should sleep in their preferred position—whether on their back, side, or stomach. While the sensors and wires may feel unusual initially, they’re designed to accommodate natural movement and position changes throughout the night.
What about their regular sleep schedule?
Patients should aim to go to bed at their customary time rather than forcing an earlier or later sleep schedule. If they normally stay up until midnight, attempting to sleep at 9 PM will likely result in difficulty falling asleep and skewed results. The sleep technologist can accommodate various sleep schedules to capture authentic data.
Can they bring personal comfort items?
Bringing familiar items enhances the ability to maintain regular bedtime habits. Patients are encouraged to pack:
- Their own pillow if it provides better comfort
- Comfortable sleepwear they typically wear
- Reading materials or devices for their pre-sleep routine
- Any white noise machines or sleep aids they normally use
What if they can’t fall asleep as usual?
Some anxiety about the unfamiliar environment is normal. The sleep technologist understands this and will give patients time to settle. Even if sleep onset takes longer than usual or sleep quality differs slightly, the study can still provide valuable diagnostic information. The monitoring equipment captures data throughout the night, regardless of how quickly sleep occurs.
What Can They Expect During the Sleep Study Night in Melbourne?
The polysomnography procedure Melbourne begins with arrival at the sleep clinic approximately 90 minutes before their usual bedtime. A Sleep Technologist greets them and shows them to a private bedroom equipped with ensuite facilities, comfortable bedding, and monitoring equipment.
The Sensor Setup Process
The sensor setup during sleep study takes approximately 45-60 minutes. The technologist applies small adhesive sensors to specific locations on the body using conductive paste or gel. Sensors are placed on the scalp to record brain waves (EEG), near the eyes to track eye movements (EOG), and on the chin to measure muscle tone (EMG). Additional sensors attach to the chest to monitor heart rhythm (ECG), elastic belts wrap around the chest and abdomen to track breathing movements, and a small clip fits on the finger to measure blood oxygen levels.
A nasal cannula sits beneath the nostrils to detect airflow, while a small microphone records snoring sounds. Leg sensors monitor any involuntary movements during sleep. The technologist ensures each sensor maintains proper contact with the skin and explains the purpose of each component.
The Monitoring Experience
Once the setup completes, patients can read, watch television, or relax until they feel ready to sleep. A low-light video camera records body position and movements throughout the night, while an intercom system allows two-way communication with the monitoring station. The Sleep Technologist observes all recordings from a separate control room and can respond quickly if sensors become dislodged or assistance is needed.
The wires connecting sensors to the monitoring equipment are long enough to allow comfortable sleeping in various positions. While movement is somewhat restricted, patients can turn over and adjust their position. If they need to use the bathroom during the night, they simply press a call button and the technologist temporarily disconnects the wires.
Morning Procedures
The monitoring continues until their typical wake time, usually allowing for 6-8 hours of recorded sleep data. The technologist removes all sensors in the morning and provides access to shower facilities to wash away any remaining adhesive residue. Most Melbourne sleep clinics offer a light breakfast before patients leave to resume their normal daily activities. The entire experience typically concludes by 6:00-7:00 AM
When and How Will They Receive Their Results?
How long does it take to get sleep study results in Melbourne?
Results typically become available within 7 to 14 days after the sleep study is completed. The Sleep Technologist who monitored the overnight recording compiles the raw data, which a sleep physician then analyzes to identify patterns, breathing disturbances, oxygen level drops, and other abnormalities. The complexity of interpreting sleep study results Melbourne requires thorough review, which explains the waiting period between the test and receiving findings.
Some Melbourne clinics may provide preliminary observations sooner, though comprehensive reports require complete analysis. Patients should ask their specific clinic about expected turnaround times during the initial consultation, as processing speeds can vary between facilities.
What happens after the data is analyzed?
The sleep physician prepares a detailed report summarizing the findings, including:
- Total sleep time and sleep efficiency percentages
- Number and severity of breathing interruptions (apnea-hypopnea index)
- Oxygen saturation levels throughout the night
- Limb movement patterns
- Sleep stage distribution
- Specific diagnosis based on observed patterns
This report is sent to the referring doctor or specialist who originally ordered the sleep study. The referring physician uses these findings alongside the patient’s medical history and physical examination results to develop a comprehensive understanding of the sleep disorder.
How is the follow-up consultation scheduled?
The clinic typically contacts patients once results are ready to schedule a follow-up appointment. This consultation usually occurs with the doctor or ENT specialist who referred them for the sleep study. Patients preparing for How to Prepare for Your Sleep Study Melbourne Appointment should anticipate this follow-up as an essential component of the diagnostic process.
During this appointment, the specialist will:
- Explain the sleep study findings in understandable terms
- Discuss how the results correlate with reported symptoms
- Present treatment options tailored to the specific diagnosis
- Answer questions about the condition and recommended therapies
- Provide prescriptions or referrals if treatment devices are needed
Can patients access their results before the consultation?
Many Melbourne sleep clinics now offer patient portals where individuals can view their reports electronically. However, interpreting sleep study results Melbourne without medical guidance can be confusing due to technical terminology and complex metrics. Click here to get more about sleep disorders.
Are There Any Risks or Precautions They Should Know About?
Is a sleep study safe?
Sleep studies Melbourne are remarkably safe procedures with minimal risks due to their completely non-invasive nature. The safety of sleep studies Melbourne ranks among the highest of any diagnostic medical tests, as no needles, medications, or surgical procedures are involved.
What discomforts might occur during the test?
The most common complaint involves mild skin irritation where adhesive sensors attach to the body. Some patients experience slight redness or itchiness at sensor sites, particularly on the scalp and face. These reactions typically resolve within hours after sensor removal.
The adhesive residue left behind can feel sticky or uncomfortable, though clinics provide shower facilities and assistance with thorough cleaning after the study. A small number of people find the sensation of wearing multiple sensors mildly claustrophobic or restrictive, though the wires allow sufficient movement for comfortable sleep positions.

How do minor discomforts compare to untreated sleep disorder risks?
The temporary inconveniences pale in comparison to the serious health consequences of undiagnosed sleep conditions. Untreated obstructive sleep apnea significantly increases the risk of:
- High blood pressure and cardiovascular disease
- Stroke and heart attack
- Type 2 diabetes
- Depression and anxiety
- Daytime accidents due to excessive sleepiness
- Reduced cognitive function and memory problems
What precautions should patients take?
Those with sensitive skin should inform the sleep technologist before the study begins. Alternative adhesive options may be available for individuals with known allergies. Patients taking blood-thinning medications can safely participate, though they should mention this during booking.
Anyone with active skin infections or open wounds near sensor placement areas should reschedule their appointment. Claustrophobic individuals benefit from discussing their concerns with staff beforehand, as technologists can explain the setup process and demonstrate how quickly sensors disconnect if needed.
How to prepare for your sleep study Melbourne appointment with safety in mind?
Arriving with clean, product-free skin ensures optimal sensor adhesion and reduces irritation risk. Avoiding caffeine and alcohol before the study not only improves test accuracy but also helps patients relax during the monitoring process.
Related : Your First Step to Quality Sleep: A Sleep Study Hobart